Macular Degeneration
What is Age-Related Macular Degeneration (AMD)?
Age-related macular degeneration (AMD) is a condition that affects the retinal cells in the macula, which is the area of the retina responsible for our central and most important vision. The cells in the macula are needed for seeing fine detail (reading and driving etc.). When macular degeneration occurs, these cells become damaged and stop functioning as well. This results in symptoms such as blurred vision and distortion. AMD specifically affects your central vision, peripheral vision typically remains normal.
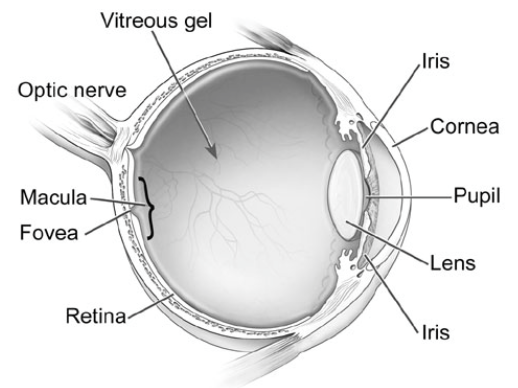
*Image courtesy of the National Eye Institute http://www.nei.nih.gov
Why do I have Age-Related Macular Degeneration?
We do not know why some people develop AMD and others do not. However, there are several known risk factors:
• Age: Your risk of developing AMD increases with age. It is most commonly seen after the age of 60.
• Family History: You have a higher risk of developing AMD if someone in your family had or has it.
• Caucasian race: AMD is much more common in Caucasians than other races.
• Poor Diet: A diet that includes few fruits and vegetables can increase your risk of AMD.
• Elevated Cholesterol
• Cardiovascular Disease
• Smoking: Smoking increases your risk of developing AMD.
What is the Difference Between Dry and Wet Age-Related Macular Degeneration?
AMD is classified as either dry or wet (also called neovascular). When AMD first develops, it begins as the dry form. If you have early changes you may not even have any symptoms, but your eye doctor can detect changes in your macula during an eye exam. Patients with AMD typically develop deposits in their macula called drusen. Development of drusen can cause mild blurring of vision and distortion, but typically does not cause a large drop in vision. If your Dry AMD progresses, you can develop advanced changes called geographic atrophy. These are areas were the actual retinal cells have degenerated and do not function any more. If geographic atrophy involves the very center of your macula, you can experience a large drop in your central vision. There is no treatment available for Dry AMD.
Wet (neovascular) AMD refers to the development of an abnormal blood vessel underneath the macular nerve tissue that leaks and bleeds. When this occurs patients often describe a sudden and dramatic onset of decreased vision and/or distortion. If this occurs, it is important that you are evaluated by your doctor as soon as possible to receive treatment to shut the abnormal blood vessel down and prevent further damage. Left untreated, the abnormal blood vessel will continue to leak and bleed causing scarring in the central macula. This will eventually destroy the central vision. Fortunately, conversion to wet AMD only occurs in about 10% of dry AMD patients.

An eye with Dry AMD showing drusen in the macula

An eye with new-onset Wet AMD (right) showing drusen with a subretinal hemorrhage.
How is AMD diagnosed?
The presence of AMD can typically be determined on clinical exam. Diagnotic testing including Optical Coherence Tomography (OCT) and Fluorescein Angiography (FA) can help determine the severity of the disease and whether it is dry or wet.
If I have Dry AMD, what can I do to decrease my chances of developing Wet AMD?
Patients with intermediate or worse Dry AMD benefit from a certain formulation of vitamins to decrease their risk of converting to Wet AMD. A large clinical trial performed by the National Eye Institute called the Age-Related Eye Disease Study 2 (AREDS2) found the following formulation most beneficial:
• Vitamin C (500 mg)
• Vitamin E (400 IU)
• Lutein (10 mg)
• Zeaxanthin (2 mg)
• Zinc (80 mg)
• Copper (2 mg)
There are many tablets available on the market that have this specific formulation. They are available over the counter without a prescription. It is important to remember that these vitamins are not a cure for Dry AMD, they only help to slow down progression of the disease. Additionally, if you don’t have any signs of macular degeneration or have very early signs of Dry AMD, there is no evidence that these vitamins will be of any benefit to you. In addition to these vitamins, if you have Dry AMD some dietary changes can help prevent further vision loss. Dietary recommendations include eating a variety of colorful fruits and vegetables, choosing healthy unsaturated fats (like those found in olive oil) over saturated fats, choosing whole grains (whole wheat bread) over refined grains (white bread) and adding fish to your diet (a good source of omega-3 fatty acids). You can also monitor for any changes yourself with an Amsler Grid. We can provide a grid for you at our office. You want to test each eye separately. Cover one eye and look at the central dot with the uncovered eye. Concerning features would be if any of the lines look bent or wavy, of if sections of the grid are blurry or missing. If you notice new any changes you should call our office right away, as this could be a sign of progression of disease.

Normal Amsler Grid

Abnormal Amsler Grid

An example of loss of central vision when looking at a clock.
If I develop Wet AMD, what is the treatment?
There is no cure for wet AMD. However, the abnormal blood vessels that develop can be shut down with medications that are injected directly into the eye. These medications include:
• Avastin (Bevacizumab)
• Lucentis (Ranibizumab)
• Eylea (Aflibercept)
Injections are typically given every 4 weeks until the blood vessel is shut down. Thereafter, the interval between injections may be increased as much as your eye can tolerate. However, you will likely need continued injections to keep the blood vessels shut down and maintain your vision. Other treatment options include Photodynamic Therapy (PDT) and laser photocoagulation. However, these treatments have fallen out of favor with the advent of the anti-VEGF medications mentioned above.
Further Information
If you have any questions or concerns regarding this or any other information please call our office at 614-464-3937.
